Mental health professionals often struggle with the time-consuming process of writing progress notes. This can lead to burnout, mistakes, and less time for patient care. AI tools now offer a solution, cutting documentation time by 72%, saving 5–10 hours per week, and improving accuracy. Here’s how AI can help:
- Automates Note Creation: Transforms session recordings into structured notes in seconds.
- Customizable Templates: Supports formats like SOAP, DAP, and BIRP for consistency.
- EHR Integration: Syncs with electronic health records and telehealth platforms.
- HIPAA Compliance: Ensures secure and private documentation.
With over 19,616 mental health professionals already using tools like Therapulse and Mentalyc, AI is transforming clinical documentation. Whether you’re looking to save time or reduce errors, these tools can help you focus more on your patients.
Common Problems with Writing Progress Notes by Hand
Writing progress notes manually can be a real struggle for mental health professionals. It affects both how practices run and the quality of care patients receive. Let’s break down the main issues with handwritten notes.
Lack of Time and Heavy Workload
Behavioral health providers often spend too much time on paperwork, which creates several problems [4]:
- Longer work hours and piles of unfinished tasks
- Less time to connect with patients, increasing burnout risk
- Delays in submitting insurance claims
Mistakes and Inconsistent Notes
Handwritten notes are prone to errors that can disrupt patient care and practice operations. Some common problems include:
- Missing or incomplete details
- Inconsistent formatting
- Important information left out
- Hard-to-read handwriting
These issues can even lead to insurance claim denials [4]. On the other hand, practices using automated systems report that 90% of notes are submitted within 24 hours [4].
Keeping Data Safe and Meeting Privacy Rules
Physical records come with serious security and compliance risks, such as:
- Easy loss or damage, with no backups
- Limited storage space
- Risk of unauthorized access and lack of proper tracking
Switching to digital tools can cut documentation time by over 70% while ensuring compliance with HIPAA requirements [4].
These challenges underscore why many mental health practices are turning to AI-powered tools to simplify documentation and improve security standards.
How AI Can Help with Progress Notes
AI tools are transforming how therapists handle documentation. By automating repetitive tasks, they save time and improve the clarity and reliability of progress notes, allowing therapists to concentrate more on patient care.
Using AI to Create Notes Automatically
AI-powered software can turn session recordings into detailed progress notes in just seconds, cutting documentation time by as much as 72% [1]. These tools analyze the session content and generate notes that cover:
- Key discussion points
- Treatment methods used
- Observations on patient progress
- Follow-up plans and action items
Tailored Note Formats for Various Practices
AI tools provide templates that cater to different documentation needs. Common options include:
| Format | Purpose |
|---|---|
| SOAP | A structured, problem-focused method often used in medical settings |
| DAP | Ideal for brief therapy sessions requiring concise documentation |
| BIRP | Focuses on behavioral health, emphasizing interventions and responses |
These formats help maintain uniformity while meeting insurance documentation standards [2].
Integration with EHR and Telehealth Platforms
AI tools simplify workflows by offering:
- Seamless integration with EHR systems for automatic note syncing
- Compatibility with telehealth platforms
- HIPAA-compliant data sharing for secure documentation
These features reduce manual data entry and create a smoother documentation process across systems [1][2].
“AI-powered tools like Behavioral Health Notes and Mentalyc use machine learning and natural language processing to generate detailed progress notes from session data, reducing the time spent on documentation by up to 72% and improving accuracy by minimizing human error” [1][2][3].
While these tools significantly streamline documentation, pairing them with effective strategies can further boost productivity.
sbb-itb-8e8938b
Tips for Writing Progress Notes Faster
Cutting down on the time spent on documentation doesn’t mean sacrificing quality. Here are some practical strategies to help you write progress notes more efficiently without compromising on detail.
Write Notes During or Immediately After Sessions
Documenting in real-time or shortly after a session helps you capture important details while they’re still fresh. This approach reduces errors and the need for later revisions. Research indicates that immediate documentation boosts both accuracy and retention of critical information [5].
Here’s how you can make this work:
- Use a laptop or tablet during sessions, or set aside 5-10 minutes afterward to jot down key points.
- With patient consent, record sessions for reference when writing your notes.
Leverage AI Tools for Session Summaries
AI tools are transforming the way therapists handle documentation. For behavioral health professionals, these tools can significantly cut down the time spent on progress notes [3].
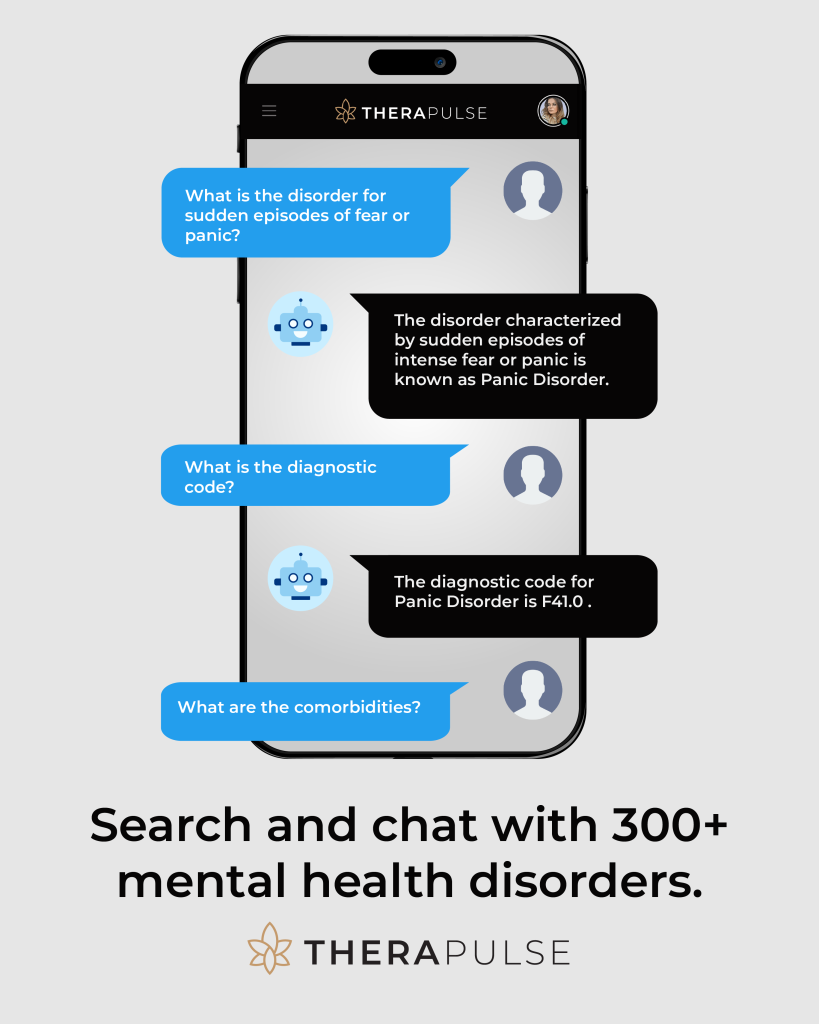
For example, Therapulse offers features that simplify the process:
| Feature | What It Does |
|---|---|
| Session Scribe | Transcribes and summarizes therapy sessions in real-time. |
| Automated Progress Notes | Creates structured notes in formats like SOAP or DAP. |
Maximize the Benefits of AI Tools
To get the most out of AI tools, consider these tips:
- Customize Templates: Adjust templates to fit your style and common treatment scenarios. For instance, Therapulse’s Professional plan includes templates tailored for various therapy types and note formats.
- Integrate with EHR Systems: Sync your AI tools with your existing electronic health records (EHR) and telehealth platforms. This eliminates duplicate data entry and ensures all records stay consistent.
- Practice Voice Commands: Many AI tools come with voice-to-text features. Regularly practicing these commands can save you time by reducing the need to type out notes manually.
How to Pick the Right AI Tool for Progress Notes
Now that we’ve looked into ways to speed up note-taking, let’s turn to selecting the best AI tool to boost your productivity.
Key Features to Look For
When choosing an AI tool for progress notes, focus on features that simplify your workflow and match your practice’s specific requirements:
| Feature | What It Does |
|---|---|
| Secure Storage | Keeps your documentation safe with encrypted backups |
| Voice Commands | Allows hands-free note-taking |
| Customizable Templates | Fits various note formats like SOAP, DAP, and BIRP |
| Advanced Analytics | Monitors your documentation habits and efficiency |
Many tools come with tiered pricing plans that include options like transcription, template customization, and secure storage. These plans typically start at around $99/month for moderate usage.
Ensure the Tool Meets Privacy Requirements
Handling patient data means privacy is non-negotiable. Look for tools that are HIPAA-compliant, offer end-to-end encryption, provide secure backups, and maintain detailed access logs. While AI tools can save therapists 5–10 hours per week [3], safeguarding patient confidentiality should always come first.
Confirm Compatibility with Your Existing Systems
To avoid workflow interruptions, check that the tool integrates smoothly with your current systems. This includes compatibility with EHRs, telehealth platforms, and billing software. Here are some integration points to consider:
| Integration | Why It’s Important |
|---|---|
| EHR Systems | Automatically syncs patient records |
| Billing Software | Simplifies administrative work |
| Calendar Tools | Helps coordinate scheduling and documentation |
Clinical Documentation and AI: A New Approach
AI technology is changing the way mental health professionals handle clinical documentation, especially progress notes. For instance, WellPower‘s use of AI-driven scribe technology has made documenting more efficient, freeing up therapists to spend more time focusing on patient care [6].
By automating repetitive tasks, AI tools address daily challenges therapists face, helping them prioritize delivering quality care. Wes Williams, CIO and Vice President of WellPower, highlights this shift:
“Clinical documentation is a promising area for AI, particularly in behavioral health” [6]
But it’s not just about saving time. Tools like Therapulse simplify the process with features like secure storage and customizable templates. They work smoothly with existing healthcare systems while adhering to HIPAA regulations, ensuring a streamlined and compliant approach to documentation.
To get the most out of these tools, therapists should integrate them thoughtfully into their workflows. This includes customizing features to suit specific needs and carefully reviewing AI-generated notes to ensure they align with clinical objectives. The combination of therapist expertise and AI-driven efficiency creates a documentation process that benefits both providers and patients.
FAQs
Here are answers to some common questions about speeding up therapy note documentation with AI tools.
What is the fastest way to write therapy notes?
One of the quickest methods is using AI-powered tools alongside structured templates like SOAP, DAP, or BIRP. Documenting immediately after sessions can also save time. Together, these strategies can cut documentation time by as much as 72% [3].
What is the best AI for writing TherapyNotes?
Here are some AI tools designed for mental health documentation:
| Tool Name | Key Features | Benefits |
|---|---|---|
| Mentalyc | Generates notes from session recordings | Offers custom templates, fast processing [2] |
| Behavioral Health Notes | Creates notes and syncs with EHRs | Simplifies workflow integration [1] |
| Therapulse | Transcribes sessions, supports various note formats | Provides advanced customization options |
When choosing an AI tool, consider factors like:
- Variety and flexibility of templates
- Compatibility with your current systems
- Ease of use and available support
- Security and compliance with regulations
Pick a tool that aligns with your workflow and documentation needs. These tools can help therapists save time while maintaining accurate and compliant records.