AI therapy notes use artificial intelligence to automatically create structured, professional documentation of therapy sessions. This technology can save therapists up to 90% of documentation time, improve accuracy, and help identify trends across sessions. Popular frameworks supported include SOAP, DAP, and BIRP formats, with seamless integration into EHR and telehealth systems.
Key Benefits:
- Time Savings: Reduces paperwork by up to 40%.
- Improved Accuracy: Captures conversations verbatim.
- Trend Analysis: Identifies patterns across sessions.
- Accessibility: Supports professionals with ADHD or dyslexia.
Challenges:
- Privacy Risks: Requires strict HIPAA compliance.
- Over-Reliance: Therapists must review AI outputs to ensure quality.
Top Tools:
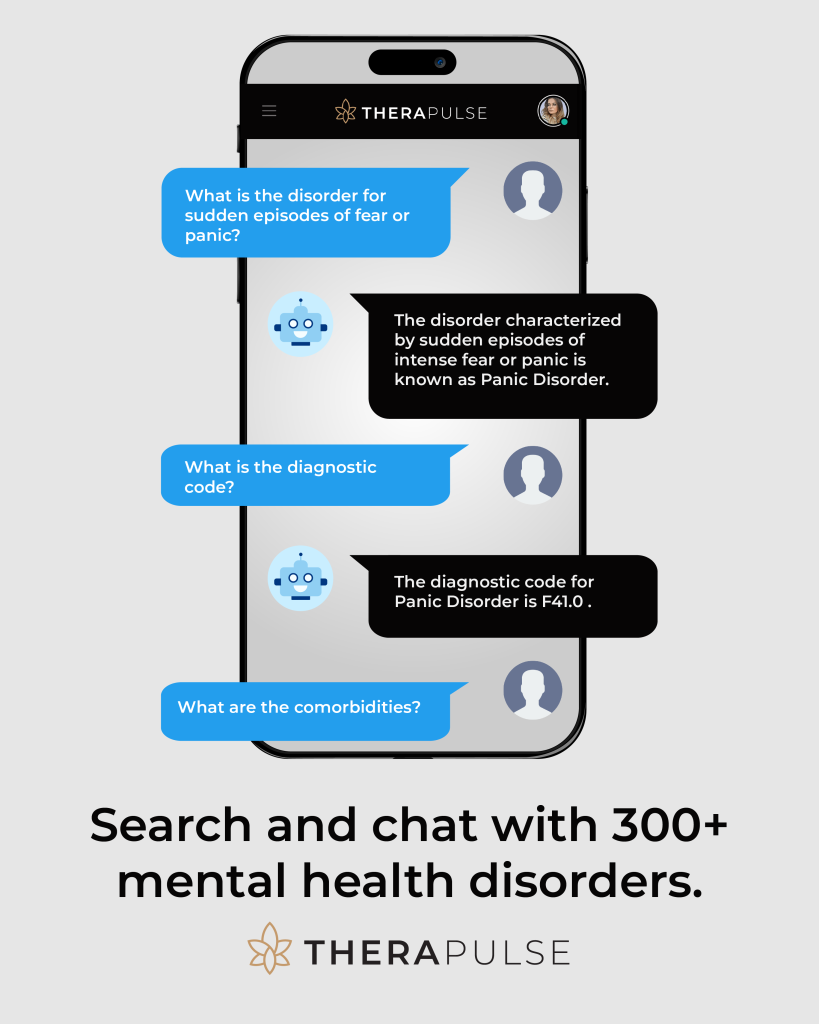
- TheraPulse: Real-time transcription, customizable note formats.
- Upheal: Therapy-specific AI models.
- Behavioral Health Notes: User-friendly with speech-to-text features.
AI therapy notes streamline administrative tasks while keeping the therapist-client connection central. Choose tools that fit your practice size, specialization, and budget while prioritizing security and ethical use.
Features and Benefits of AI Therapy Notes
How AI Generates Notes Automatically
TheraPulse’s Session Scribe uses real-time transcription to turn therapy sessions into structured, professional notes. It captures key elements of the conversation and organizes them into documentation that aligns with clinical standards – all in an instant.
Flexible Note Formats
Modern AI tools for therapy notes adapt to various documentation styles, catering to different therapeutic methods and institutional needs. They support popular frameworks like:
| Format | Primary Focus |
|---|---|
| SOAP | Focuses on a structured, problem-solving method |
| DAP | Centers on description, assessment, and planning |
| BIRP | Highlights behavior-focused interventions |
Behavioral Health Notes, for instance, allows therapists to switch between these formats without losing consistency in their records [4]. Combined with real-time note generation and seamless integration, this adaptability makes documentation smoother and more efficient for mental health professionals.
Integration with EHR and Telehealth Systems
AI-powered therapy notes work effortlessly with existing healthcare systems. Therapedia’s platform, for example, connects securely with major Electronic Health Record systems and complies with HIPAA standards [2]. It automates the integration of notes into patient records, supports secure data sharing, and simplifies workflows.
“Within six months of adoption, we achieved a 40% reduction in documentation time while maintaining higher accuracy in our clinical notes” [2].
These integrations not only improve efficiency but also free up valuable time for therapists to focus on their clients. However, they also bring up critical questions about privacy and ethics, which will be discussed in the next section.
Challenges and Ethical Issues
Privacy and Security Risks
Even with encryption and access controls in place, ensuring data security while integrating systems smoothly can be a tough balancing act. Protecting client information and maintaining trust are non-negotiable priorities. Here are some critical measures:
| Security Measure | Purpose |
|---|---|
| Data Encryption | Safeguards sensitive information during storage and transmission |
| Access Controls | Restricts system access to only authorized personnel |
| System Maintenance | Preserves system integrity and tracks all data interactions |
Platforms like Therapedia have adopted advanced encryption methods and strict access protocols that comply with HIPAA standards [2]. Additionally, practitioners must secure informed consent from clients when incorporating AI into documentation processes.
While these measures help protect data, there’s another concern: over-reliance on AI could potentially undermine the quality of care.
Over-Reliance on AI
Therapists need to actively review and refine AI-generated notes to ensure they capture the nuances of each client’s situation. Relying too heavily on AI can lead to:
- Overlooking subtle client behaviors or cues
- Misinterpreting cultural or contextual factors
- Losing the personal touch essential for effective therapy
To address these risks, therapists should:
- Review and refine AI outputs: Check automated notes for accuracy and completeness.
- Add personal insights: Incorporate unique observations that AI might miss.
- Document contextual details: Include information that reflects the client’s specific circumstances.
“The therapeutic relationship remains the cornerstone of effective mental health treatment. AI should enhance, not diminish, this fundamental aspect of care” [1].
Choosing the Right AI Therapy Notes Tool
Selecting the right AI therapy notes tool is essential for ensuring your practice runs smoothly while maintaining ethical standards and client care.
Key Features to Consider
When evaluating AI therapy notes tools, focus on these critical features:
| Feature Category | What to Look For |
|---|---|
| Security & Compliance | HIPAA-compliant systems, encryption, and secure access controls |
| Functionality | Customizable templates, EHR integration, telehealth support |
| Performance | Accurate transcription and advanced language processing |
| Usability | Easy-to-navigate interface with minimal training required |
| Support | Access to training materials and responsive technical help |
Comparison of Leading AI Tools
Let’s take a closer look at some of the top AI therapy note tools and their standout features:
- TheraPulse: Offers pricing tiers ranging from $29 to $149/month, depending on session volume. Features include automated progress notes, session transcription, and the NeuroSearch Chatbot (available in the Professional tier).
- Upheal: Focuses on therapy-specific AI models to create accurate, original content for documentation [3].
- Behavioral Health Notes: Known for its straightforward approach, it includes shorthand entries, customizable checkboxes, and integrated speech-to-text functionality [4].
Research shows that AI tools can save therapists 6–10 hours per week on documentation [3]. To choose the best platform, consider these factors:
| Consideration | Impact |
|---|---|
| Practice Size | Determines the pricing tier and session volume needed |
| Specialization | Influences the types of notes and customization required |
| Tech Comfort | Affects the level of training and support necessary |
| Budget | Limits the range of tools and features you can afford |
Opt for a platform that aligns with your practice’s workflow while safeguarding client data. A trial period can be a great way to ensure the tool meets your specific needs.
Next, we’ll dive into how to effectively implement and use AI therapy notes in your practice.
sbb-itb-8e8938b
Using AI Therapy Notes Effectively
Using AI for therapy notes can significantly ease administrative tasks while ensuring care quality remains high.
Steps for Implementation
| Phase | Key Actions | Expected Outcomes |
|---|---|---|
| Planning | • Identify workflow needs and define success metrics • Choose an AI tool that fits your practice |
Clear plan for execution |
| Setup | • Configure system settings • Integrate with your EHR • Validate data security measures |
Fully functional platform |
| Training | • Conduct staff training with workshops and sample scenarios • Establish support resources |
Confident, well-prepared team |
| Launch | • Start with a pilot group • Monitor performance closely • Collect and act on feedback |
Smooth, validated rollout |
Adopting AI can save up to 40% of documentation time in the first month [2]. For instance, starting with TheraPulse’s Starter plan (30 sessions per month) allows your team to adapt gradually without compromising care quality.
After implementation, sticking to effective practices ensures sustained success and reliable documentation.
Best Practices for Using AI
To maintain high-quality documentation, focus on these practices:
- Regular Quality Checks: Review AI-generated notes promptly to ensure accuracy.
- Security and Compliance: Protect client data by adhering to HIPAA standards, using encryption, secure logins, and conducting regular audits.
- Balancing AI and Human Oversight: Combine AI efficiency with human expertise by customizing templates, reviewing notes, and making necessary adjustments.
“AI-powered progress notes are designed to enhance the therapist’s efficiency without compromising the quality and accuracy of the documentation.” – Behavioral Health Notes [4]
Clear documentation guidelines are also critical for consistency:
- Documentation Standards: Establish approval processes for notes. Tools like TheraPulse offer multiple formats (SOAP, DAP, BIRP) to help maintain uniform documentation across your practice.
The Future of AI in Mental Health Documentation
AI is changing the way mental health documentation is handled, making processes smoother and helping therapists achieve better outcomes.
Advances in AI for Therapy Notes
Technologies like natural language processing (NLP) and machine learning are reshaping how therapy notes are created. NLP goes beyond simple transcription by understanding the context of therapy discussions, while machine learning helps spot trends and even predict treatment results. These tools are evolving to grasp the nuances of therapy-specific language, offering deeper insights for mental health professionals [2].
| Technology | Current Use | Future Potential |
|---|---|---|
| Natural Language Processing | Generating and transcribing notes | Understanding therapy-specific nuances |
| Machine Learning | Identifying patterns | Recommending treatments, assessing risks |
| Predictive Analytics | Tracking outcomes | Forecasting treatment results using data |
How AI Benefits Clients
AI tools are helping therapists improve client care by offering real-time insights, spotting behavioral trends, and refining treatment plans. For example, Mentalyc‘s AI scribe allows clinicians to spend less time on documentation and more time engaging with clients [5]. Practices using AI note generators have seen a 40% drop in the time spent on paperwork [2], freeing up therapists to focus on their clients.
These tools build on the accuracy and efficiency of current AI systems, making them even more valuable for mental health professionals. While AI continues to evolve, its role is to assist – not replace – therapists, ensuring that the human connection remains at the heart of mental health care. This progress paves the way for the next wave of documentation tools designed to support clinicians and their clients alike.
Conclusion and Recommendations
Key Takeaways
AI therapy notes have reshaped mental health documentation by reducing paperwork time by 40% and improving care quality [2]. These tools help therapists focus more on their clients by simplifying documentation, safeguarding data, and offering insights that can refine treatment plans. Platforms like TheraPulse showcase how AI can handle tasks like session transcription and secure, HIPAA-compliant data storage.
The growing adoption of AI therapy notes shows their value in modern mental health practices. However, success depends on careful and thoughtful integration into daily workflows.
Practical Advice
AI is changing how mental health documentation is done, but it’s essential to use these tools in a way that supports, not replaces, the therapist’s expertise.
“AI therapy notes can help by allowing therapists to focus more on client care, providing more accurate and consistent documentation, and enabling the identification of patterns and insights that can inform treatment plans” [1][2].
To get the most out of these tools, mental health professionals should:
- Double-check AI-generated notes for accuracy.
- Balance automation with personal judgment.
- Choose tools that meet HIPAA compliance standards [4].
The aim is to use AI for its efficiency while keeping the human connection central to mental health care. By striking this balance, therapists can streamline their work without compromising the quality of client care.