Writing a biopsychosocial assessment doesn’t have to be complicated. This tool helps mental health professionals evaluate a client’s well-being by looking at biological, psychological, and social factors. Here’s what you need to know:
- What it is: A detailed assessment that examines physical health, mental health, and social influences to create personalized treatment plans.
- Key components: Include client demographics, medical and mental health history, family dynamics, support systems, and substance use patterns.
- Structure: Use the “5 P’s” framework – Presenting Problem, Predisposing Factors, Precipitating Factors, Perpetuating Factors, and Protective Factors.
- Tools and templates: Simplify documentation with structured templates and AI tools for accuracy and efficiency.
This guide explains how to gather and organize information, document findings clearly, and use templates to streamline the process.
The Biopsychosocial Model Explained
Dr. George Engel introduced the biopsychosocial model as a way to understand how biological, psychological, and social factors work together to influence mental health [1].
Biological Factors in Mental Health
Biological factors focus on the physical aspects of mental health, including:
- Neurological and genetic influences, such as brain chemistry and inherited traits
- Physical health conditions, including chronic illnesses
- Medical history, covering past treatments and health issues [2][3]
For instance, chronic conditions like diabetes or heart disease can worsen mental health challenges like anxiety or depression.
Psychological Factors in Mental Health
The psychological aspect examines mental and emotional influences on well-being. This includes:
- Cognitive and emotional processes, like thought patterns and coping skills
- Mental health history, including previous diagnoses
- Personal beliefs and attitudes [1][4]
Unhelpful thought patterns, for example, can make recovery more difficult and intensify mental health struggles.
Social Factors in Mental Health
Social influences, such as family dynamics, financial stability, living environment, and cultural background, play a key role in shaping mental health. These factors affect access to resources, emotional support, and stress management [2][3]. A strong support system can improve resilience and aid in recovery.
This model helps clinicians consider all aspects of a person’s life when assessing their mental health, allowing for a well-rounded approach to treatment planning. By addressing biological, psychological, and social factors, clinicians can create more effective and personalized care strategies.

Main Parts of a Biopsychosocial Assessment
This section breaks down how to structure and document a thorough biopsychosocial assessment based on the biopsychosocial model.
Key Components
A well-rounded assessment includes the following sections:
- Basic Client Information
Record details like demographics, referral source, the main issue the client is facing, and their treatment goals. - Biological Assessment
Include information about physical health, such as medical conditions, genetic risks, and medication history [1]. - Psychological Assessment
Document mental health symptoms, diagnoses, treatments, and coping strategies [2]. - Social Assessment
Note support networks, living environment, employment situation, and cultural considerations [3].
Organizing with the 5 P’s
The 5 P’s framework helps organize assessment findings into a clear structure:
| Component | Description |
|---|---|
| Presenting Problem | The main issue at hand |
| Predisposing Factors | Past influences contributing to the issue |
| Precipitating Factors | Recent events or triggers |
| Perpetuating Factors | Ongoing elements maintaining the problem |
| Protective Factors | Strengths and resources available |
Documenting and Combining Information
Each section should capture observations, history, current status, and how these elements affect the client’s functioning. Keep documentation clear, objective, and professional [1][4]. The goal is to combine biological, psychological, and social aspects into a unified understanding of the client’s situation, guiding treatment planning [2].
With these elements outlined, the next step is gathering the necessary details to start the assessment process.
Collecting Basic Client Information
Gathering basic client information is the starting point for a biopsychosocial assessment. This step lays the groundwork for understanding the biological, psychological, and social factors influencing the client.
Key Information to Gather
Here are the main categories of information to collect:
| Category | Details to Collect | Purpose |
|---|---|---|
| Personal Demographics | Name, date of birth, gender, marital status | Establishes client background |
| Contact Information | Phone, email, address, emergency contacts | Ensures reliable communication |
| Insurance/Payment | Coverage details, policy numbers, payment preferences | Handles administrative needs |
| Referral Details | Source, reason for referral, previous providers | Provides context for the referral |
| Legal Status | Current legal issues, guardianship, power of attorney | Identifies legal factors |
Best Practices for Documentation
To protect client privacy and ensure consistency, use standardized intake forms and electronic health records. These tools not only help maintain HIPAA compliance but also improve the accuracy and accessibility of data [1][4].
Why This Information Matters
The details collected at this stage directly influence treatment planning, communication among care providers, and culturally aware interventions [1][3][4]. Missing or incorrect information can lead to misunderstandings, ineffective treatment plans, and strained therapeutic relationships [1][4].
Take the time to cross-check information and approach the process with cultural sensitivity to encourage honest and accurate sharing. Once this step is complete, you can move on to reviewing the client’s medical and mental health history for a more comprehensive understanding of their needs.
Documenting Medical and Mental Health History
Keeping a detailed record of medical and mental health history is crucial for understanding how biological and psychological factors impact a client’s current condition. This approach aligns with the biopsychosocial model by addressing both physical and mental aspects thoroughly.
Key Components of Medical History
| Component | Details | Importance |
|---|---|---|
| Chronic Conditions | Current illnesses, past surgeries, hospitalizations | Identifies major health challenges |
| Medications | Current prescriptions, dosages, duration of use | Evaluates medication effects |
| Family Health | Hereditary conditions, family medical history | Highlights potential genetic health risks |
| Physical Symptoms | Current symptoms, onset patterns, severity | Links physical and mental health issues |
Mental Health History Details
Capturing mental health history involves documenting both past experiences and current symptoms [1].
Previous Mental Health Treatments
- Diagnoses and their outcomes
- Past therapy experiences
- Responses to previous treatments
- Records of hospitalizations
Current Mental Health Status
- Present symptoms and their severity
- Effectiveness of ongoing treatments
- Recent changes in mood, behavior, or cognition
- Current coping strategies
Combining Physical and Mental Health Records
Research shows that over 55% of adults with chronic pain also report symptoms of anxiety and depression [1]. Combining physical and mental health records ensures a more complete understanding of the client’s needs.
Best Practices for Documentation:
- Use precise, professional language
- Include specific dates and timeframes
- Note symptom patterns and treatment outcomes
- Record any adverse reactions or side effects
Assessing Protective Factors
It’s also important to document elements that support resilience, such as strong support systems, past achievements, and positive lifestyle changes.
Once the medical and mental health history is recorded, the next step is to explore the client’s social and life history for a fuller understanding.
Understanding Social and Life History
Social and life history shed light on the factors shaping mental health, including relationships, living conditions, and past experiences. These elements work alongside biological and psychological factors to influence overall well-being.
Key Areas of Social Assessment
| Domain | Assessment Focus | Clinical Relevance |
|---|---|---|
| Family Dynamics | Family relationships and support | Highlights potential stressors and resources |
| Living Situation | Housing stability and safety | Helps evaluate environmental impacts |
| Education & Work | Education, job history, and satisfaction | Provides insight into daily functioning |
| Support Systems | Social networks and resource access | Identifies available support systems |
Family Background Assessment
Understanding family background is essential for identifying both stressors and sources of support. Focus on areas such as:
- Family composition and relationships
- Communication styles within the family
- Cultural traditions and values
- History of mental health within the family
- Attitudes toward mental health treatment
Educational and Occupational History
Education and work experiences play a major role in shaping mental health. Factors like academic success, workplace satisfaction, and managing work-life balance contribute to stress levels and self-esteem. Key areas to explore include:
- Past educational achievements and challenges
- Career progression and goals
- Workplace dynamics and relationships
- Time management and organizational skills
Support Network Analysis
Support networks are vital for mental health. These include family, friends, healthcare providers, and community groups. Assess both the availability and quality of support in areas such as:
- Access to healthcare services
- Involvement in faith-based or community groups
- Connections within the neighborhood
- Participation in social or recreational activities
- Engagement with online communities
Cultural Considerations
Cultural background shapes how individuals view family roles, communication, and mental health care. It’s important to consider:
- Family roles and expectations
- Preferred communication styles
- Use of traditional healing methods
- Influence of spiritual or religious beliefs
Assessing Substance Use and Addictions
Evaluating patterns of substance use and addiction is crucial for crafting effective treatment plans. According to SAMHSA, about 20.3 million people aged 12 or older faced substance use disorders in 2020, emphasizing the importance of thorough assessments [1].
Key Assessment Components
| Assessment Area | Information to Gather | Clinical Significance |
|---|---|---|
| Substance History | Type, frequency, duration of use | Helps determine severity and treatment needs |
| Usage Patterns | Method of consumption, triggers | Identifies risk factors and intervention points |
| Treatment History | Previous interventions, outcomes | Guides the choice of effective approaches |
| Impact Areas | Health, relationships, work | Shows the extent of substance use effects |
Substance use disorders often result from a combination of biological predispositions, psychological stress, and social factors. This complexity makes them a critical area for biopsychosocial assessments [2][3].
Treatment History Analysis
Examining past treatment efforts provides valuable insights for current strategies. Key points to review include:
- Types of treatment programs previously tried
- Duration and completion of past interventions
- Factors that contributed to either success or relapse
Cultural Factors in Assessment
Cultural considerations are essential when assessing substance use. They can influence:
- Community attitudes toward substance use and recovery
- Traditional healing methods relevant to treatment
- Availability of culturally specific treatment resources
- Local recovery support systems
Documentation Guidelines
Use clear, professional documentation practices with standardized tools. Gather objective data while ensuring HIPAA compliance and addressing the client’s unique circumstances [4].
Once substance use and its effects are documented, the next step involves creating a structured biopsychosocial template to organize these findings effectively.
How to Build a Biopsychosocial Assessment Template
A well-designed template helps capture all biopsychosocial factors systematically. This approach not only improves efficiency but also supports personalized treatment plans tailored to each client’s needs.
Key Components of the Template
Here’s a breakdown of the main sections every biopsychosocial assessment template should include:
| Section | Key Elements | Purpose |
|---|---|---|
| Basic Information | Demographics, referral source, presenting problem | Provides context and highlights initial concerns |
| Medical History | Current/past conditions, medications, treatments | Tracks health factors influencing mental state |
| Mental Health | Previous diagnoses, treatments, hospitalizations | Documents psychological history |
| Social History | Family dynamics, relationships, support systems | Examines environmental influences |
| Substance Use | Usage patterns, treatment history, impact areas | Assesses addiction-related aspects |
Structuring the Template
Use the 5 P’s framework to organize the assessment:
- Presenting problems: What brought the client in?
- Predisposing factors: Underlying vulnerabilities or risks.
- Precipitating factors: Recent events or triggers.
- Perpetuating issues: Ongoing challenges that sustain the problem.
- Protective strengths: Skills, resources, or support systems that can aid recovery.
This structure ensures thorough and consistent evaluations, minimizing the risk of missing critical details.
Incorporating Cultural Considerations
To provide care that respects individual backgrounds, include sections that address:
- Cultural identity and practices
- Spiritual beliefs or traditional healing methods
- Language preferences and community networks
These additions help create a more inclusive and respectful assessment process.
Facilitating Team Collaboration
The template should support teamwork by including:
- Sections for treatment recommendations and planning
- Risk assessment tools
- Space for documenting progress notes and outcomes
- Care coordination details (e.g., referrals, consultations)
For instance, a psychiatrist can update medication notes while a therapist logs behavioral strategies. This shared documentation keeps everyone on the same page, improving overall care.
Finally, using AI tools can streamline the process, helping maintain accuracy and consistency in record-keeping without sacrificing quality.
Organizing the Template
Creating a well-structured template is key to using the biopsychosocial model effectively in clinical settings. A clear, logical layout helps ensure efficient and thorough documentation.
Template Structure
Divide the template into main sections like Basic Info and Medical History, with subsections for detailed notes and prompts. Start with identifying details, then move to presenting problems, historical data, current functioning, and finish with treatment recommendations. This flow keeps the documentation process smooth and organized.
Documentation Standards
Use clear formatting and standardized response fields to make the template consistent and easy to read. Separate objective details from subjective observations, and ensure it complies with HIPAA by implementing proper security measures [4]. Tailor the template for specific groups, such as older adults or pediatric clients, to meet their unique requirements.
Team Collaboration
Design the template to encourage teamwork by including sections for treatment recommendations, progress updates, and care coordination notes. Add required fields, validation prompts, and areas for supervisor reviews to ensure the documentation is accurate and complete.
A well-organized template allows clinicians to focus on using precise, professional language to document their findings effectively.
Using Clear and Professional Language
Professional documentation relies on precise, accessible language to effectively convey client information while adhering to clinical standards. This ensures the biopsychosocial model is communicated clearly, promoting collaboration and client-focused care.
Writing for Diverse Audiences and Cultures
Your biopsychosocial assessment might be read by a variety of stakeholders, including healthcare providers, insurance companies, legal professionals, and clients themselves. To ensure clarity and inclusivity, keep these principles in mind:
- Use detailed, professional, and neutral language.
- Provide explanations for technical terms when necessary.
- Choose terminology that reflects the client’s cultural and familial background.
- Replace stigmatizing language with neutral, descriptive alternatives.
- Consider cultural context when describing behaviors or symptoms.
For instance, instead of writing something stigmatizing, say: “The client has a history of substance use that has affected their mental and emotional well-being.”
Balancing Detail and Clarity
Here’s how you can reframe clinical phrases into clearer, more professional alternatives:
| Instead of Writing | Professional Alternative |
|---|---|
| “Exhibits paranoid ideation” | “Expresses ongoing concerns about others’ intentions” |
| “Poor insight and judgment” | “Displays limited awareness of consequences” |
| “Non-compliant with meds” | “Struggles with medication adherence” |
| “Presents with flat affect” | “Displays limited emotional expression” |
Documentation Best Practices
When documenting observations and findings, consider the following:
- Focus on observable behaviors and factual details; avoid personal opinions.
- Use consistent terminology throughout the assessment.
- Provide context for clinical observations to ensure clarity.
- Include relevant background information to support your findings.
“When clients can understand their own assessments, they are more likely to be engaged in their treatment plans and to adhere to recommended interventions.”
Using clear, professional language not only ensures accurate documentation but also helps create a foundation for effective and actionable care plans.
Covering All Key Areas
A biopsychosocial assessment is most effective when it captures the full picture of a client’s mental health. By examining the interplay between biological, psychological, and social factors, this approach helps identify the root causes and influences on mental health outcomes.
Key Areas to Address
To ensure your assessment is thorough, focus on these core domains:
| Domain | Key Details to Include |
|---|---|
| Biological | • Family medical history • Current health conditions • Brain chemistry considerations • Physical health evaluation • Past and present medications |
| Psychological | • Emotional regulation abilities • Cognitive patterns • Coping strategies • Mental health history • Experiences with trauma |
| Social | • Family dynamics • Support systems • Economic challenges • Workplace or school influences • Cultural background and beliefs |
Using a Structured Framework
The 5 P’s framework, previously outlined, helps ensure all critical areas are explored. Use this structure to gather detailed insights into the presenting issues, contributing factors, and available support systems for effective treatment planning [4].
Don’t Overlook These Areas
When conducting your assessment, make sure to include:
- Cultural and economic factors that may shape care approaches or symptom expression
- Environmental conditions impacting daily life
- Substance use and its potential effects
- Risks and safety concerns that may require immediate attention
Building a Complete Profile
Combine data from interviews, assessments, and client records to build a well-rounded profile. This method ensures that biological, psychological, and social factors are fully considered during treatment planning.
Tools like AI can also assist in organizing and streamlining the process, making it easier to manage complex assessments efficiently.

Using AI Tools to Simplify Documentation
AI tools are changing the game for clinicians when it comes to documenting biopsychosocial assessments. They make the process quicker and more precise, ensuring that biological, psychological, and social factors are captured effectively.
Cutting Down on Admin Time
A study by the American Psychological Association found that clinicians spend around 30% of their time on administrative tasks [1]. AI can help reduce this burden, allowing more time for patient care, by offering:
- Faster Documentation: Automated data entry and pre-filled templates speed up the process.
- Integrated Assistance: Real-time prompts and smooth data integration help ensure thorough and complete documentation.
Improving Accuracy and Consistency
AI tools help keep documentation clear and error-free. Here’s how:
| Feature | How It Helps |
|---|---|
| Quality Checks | Flags inconsistencies or mistakes. |
| Standardized Language | Encourages clear and objective terms. |
Supporting Clinical Decisions
AI goes beyond documentation. It can analyze patterns, link symptoms, recommend treatments based on evidence, and track patient progress over time. This extra layer of insight supports better decision-making for clinicians.
Tips for Using AI Effectively
- Choose platforms that align with your systems, meet HIPAA requirements, and prioritize data security.
- Use AI as a tool to assist – not replace – your expertise. Regularly review AI-generated outputs for accuracy.
How AI Improves Documentation
AI tools are changing the way biopsychosocial assessments are documented, making the process more accurate and efficient. According to the American Medical Association, healthcare providers spend around 44% of their time on administrative tasks [1]. Here’s how AI helps tackle this challenge:
Smart Automation and Error Reduction
AI can automatically fill in standard fields like demographics and medical history, cutting down on repetitive tasks. It also flags inconsistencies and ensures data accuracy by spotting errors, enforcing consistent terminology, and validating logical connections across the assessment.
Uncovering Patterns and Insights
By analyzing both past and current data, AI identifies patterns across biological, psychological, and social factors. This capability helps clinicians better understand the connections between these domains, leading to more effective treatment plans rooted in the biopsychosocial model.
Saving Time Without Sacrificing Quality
AI tools like voice-to-text transcription, customizable templates, and automated coding streamline the documentation process. These features free up clinicians to spend more time with patients while still maintaining high-quality records.
Data Security and Privacy
AI documentation systems are designed to comply with HIPAA standards, ensuring patient data is stored securely and handled with strict privacy protocols. This balance between convenience and confidentiality is critical in healthcare.
Supporting Clinical Decisions
AI enhances clinical decision-making by analyzing data, suggesting treatments backed by evidence, tracking patient progress, and identifying response trends. These tools provide actionable insights while preserving the personalized nature of care.
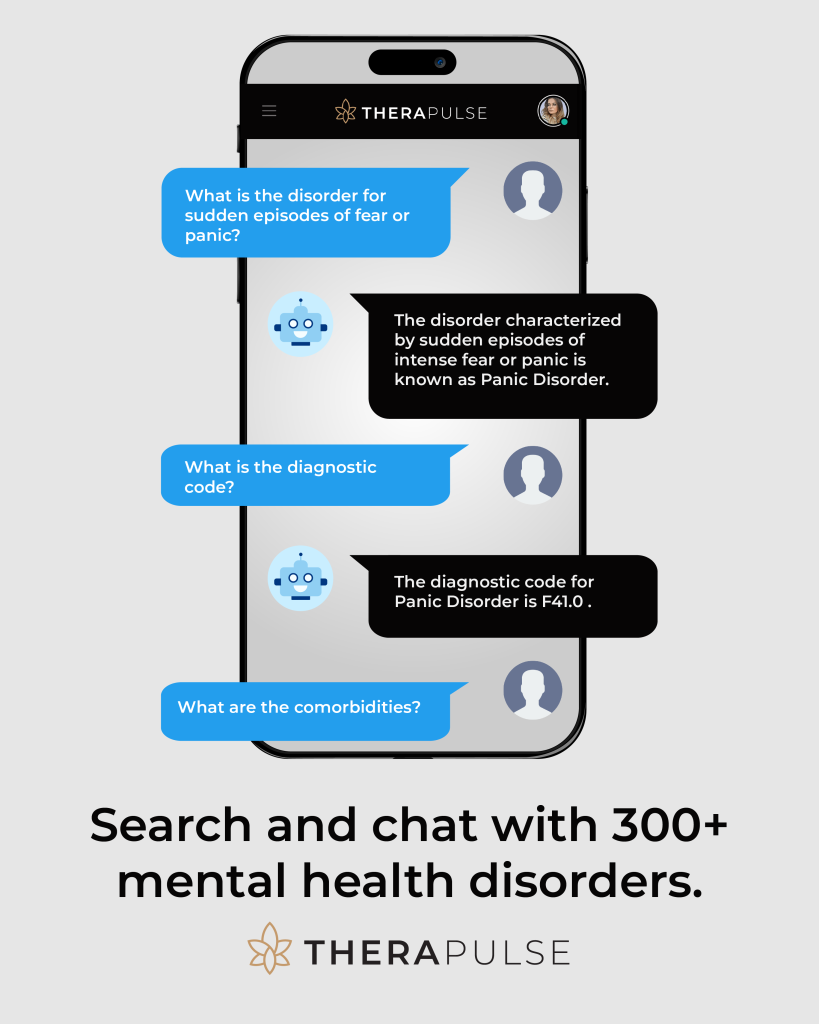
Therapulse Features for Mental Health Professionals
Therapulse harnesses AI to simplify documentation, offering tools specifically tailored for mental health professionals working on biopsychosocial assessments.
Documentation Made Simple
With tools like Session Scribe, Therapulse transcribes therapy sessions in real time. It also generates progress notes automatically, following widely used formats such as SOAP and DAP. This means clinicians can focus on their clients without worrying about missing essential details in their records.
Flexible Assessment Templates
Therapulse includes templates that can be customized to fit specific needs. With modular sections and adjustable fields, these templates integrate smoothly with EHR systems. They help ensure thorough and consistent documentation of biological, psychological, and social factors.
Strong Data Security
Client data is protected with HIPAA-compliant measures, including 256-bit encryption, secure cloud storage, and strict access controls.
Research and Efficiency Tools
The NeuroSearch feature connects clinicians to the latest evidence-based research, making it easier to include current best practices in assessments. Alongside this, other time-saving tools enhance documentation efficiency without sacrificing accuracy.
Therapulse offers pricing options to accommodate practices of all sizes, helping both new and experienced professionals streamline their work. By automating key tasks, it ensures clinicians can efficiently document the critical elements of biopsychosocial assessments with ease and precision.
Summary of Key Points
A biopsychosocial assessment looks at biological, psychological, and social factors to provide a well-rounded picture of mental health [1][5].
Here are the main components of a biopsychosocial assessment:
| Component | Purpose | Key Details |
|---|---|---|
| Basic Information | Identifies the client and context | Includes demographics, referral reasons, and presenting issues |
| Medical Assessment | Evaluates physical health factors | Covers current conditions, medications, and family medical history |
| Psychological Evaluation | Examines mental health status | Focuses on symptoms, past treatments, and coping strategies |
| Social Assessment | Considers environmental factors | Looks at family relationships, support systems, and cultural background |
Using structured templates helps ensure assessments are detailed and well-organized [4]. These templates promote consistency and cover all critical areas.
Protective factors, like strong support networks or a stable work history, play an important role in crafting effective treatment plans [4]. This method emphasizes how biological, psychological, and social factors are interconnected [5][6].
The biopsychosocial model represents a move toward more comprehensive mental health care. It recognizes the need to address the complex relationships between physical health, mental well-being, and social environment [5][3].
FAQs
What is an example of a biopsychosocial summary?
For a client dealing with depression:
- Biological: Family history of depression, current medications, disrupted sleep patterns.
- Psychological: Negative thought patterns, limited coping strategies.
- Social: Recent divorce, strained relationships, workplace challenges.
These elements work together to influence the client’s overall experience. For instance, chronic pain (biological) paired with a divorce (social) might heighten feelings of hopelessness (psychological). Addressing all three areas is crucial for creating a well-rounded and personalized treatment plan.