PIE notes are a simple and structured way to document mental health sessions. They focus on three key sections:
- Problem: The client’s challenges and symptoms (e.g., anxiety, observable behaviors).
- Intervention: Actions taken during the session (e.g., CBT techniques, assigned homework).
- Evaluation: Assessing progress and planning next steps (e.g., client’s response, future goals).
This format ensures clear, concise records that help track client progress, meet compliance standards, and improve treatment planning. Tools like templates and AI can make writing PIE notes faster and more efficient. Below, you’ll find examples, templates, and tips for writing effective PIE notes.
Breaking Down the Parts of PIE Notes
Understanding the structure of PIE notes is crucial for mental health professionals aiming to create clear and effective documentation. Let’s dive into each section to ensure thorough and objective records of client sessions.
The Problem Section
This section focuses on capturing the client’s current challenges in a clear and objective manner. It includes observable behaviors (like pacing, fidgeting, or avoiding eye contact), client-reported concerns, and assessment findings.
Key points to document:
- The client’s presenting symptoms and concerns
- Any changes since the previous session
- Observable behaviors during the session
- How the issues affect their daily life
Use factual language and avoid subjective interpretations. For example, instead of saying, “client seemed upset”, write, “client exhibited rapid breathing and reported feeling overwhelmed by work responsibilities” [2]. This approach ensures the information is actionable and supports effective treatment planning.
The Intervention Section
Here, you’ll detail the actions taken during the session to address the identified problems. It’s important to connect these actions directly to the client’s concerns.
Include details such as:
- The therapeutic techniques applied during the session
- The reasoning behind choosing these interventions
- Homework assignments or resources provided
For instance, if you used CBT techniques like relaxation exercises or thought recording, document these steps to show how the interventions were purposeful and targeted [2].
The Evaluation Section
This section focuses on assessing the effectiveness of the session’s interventions and outlining the next steps in the treatment process.
Key elements to include:
- The client’s response to the session
- Progress made toward treatment goals
- Any changes in symptoms
- Plans for future sessions or follow-ups
How It All Comes Together
Here’s an example of how these sections might look in practice:
| Section | Documentation Example |
|---|---|
| Problem | Client presented with heightened anxiety symptoms, reporting increased worry about work commitments and sleep disturbances. |
| Intervention | Implemented CBT techniques focusing on stress management and cognitive restructuring; provided relaxation practice homework. |
| Evaluation | Client demonstrated understanding of relaxation techniques and reported decreased anxiety following the session; scheduled a follow-up to review progress. |
PIE Note Examples and Templates
Sample PIE Note
Here’s an example of a well-structured PIE note that aligns with clinical documentation standards:
| Section | Content |
|---|---|
| Problem | The client reported heightened anxiety symptoms, including increased worry about work commitments and trouble sleeping. Observable behaviors included rapid speech, hand fidgeting, and difficulty maintaining eye contact. The client also mentioned missing two workdays last week due to anxiety. |
| Intervention | Used CBT techniques to address stress and restructure negative thought patterns. Introduced progressive muscle relaxation exercises during the session. Provided the client with an anxiety tracking worksheet and sleep hygiene tips as homework. |
| Evaluation | The client actively participated in relaxation exercises, noting reduced muscle tension by the end of the session. They showed a solid grasp of the CBT concepts discussed. Next steps: Continue focusing on anxiety management techniques and review the client’s sleep log in the following session. |
Writing detailed PIE notes can take time, but using templates can simplify the process, making documentation faster and more consistent.
Using Templates for Efficiency
Templates help streamline the creation of PIE notes, ensuring they are clear, concise, and meet clinical standards. Many EHR systems, like Simple Practice and Supanote, can even auto-fill client information and suggest interventions based on prior outcomes [4].
Key Template Features:
- Dropdown menus and prompts for common problems, interventions, and key details
- Pre-formatted sections for outlining treatment goals
- Integration with broader treatment plans
Tips for Effective Templates: Good templates should include clear prompts, space for observations, and fields to track progress toward goals. These features make documentation more manageable while ensuring thorough and accurate records in your clinical practice.
How PIE Notes Help Mental Health Professionals
Clearer Documentation
PIE notes break down complex client details into concise, easy-to-understand records. This structured format not only organizes information logically but also aligns with professional standards, making it easier for mental health teams to communicate and stay compliant with HIPAA regulations.
Here’s why they’re effective:
- Logical Organization: Clearly outlines client issues, actions taken, and results.
- Better Progress Tracking: Makes it easier to follow a client’s journey and care outcomes.
- Improved Team Communication: Helps providers quickly grasp client situations and updates.
Simplified Work Processes
PIE notes help simplify the documentation process, freeing up time for professionals to concentrate on their clients rather than paperwork. This is especially useful in fast-paced clinical settings, where managing time effectively is critical.
The structured approach offers these practical benefits:
| Benefit | Impact on Practice |
|---|---|
| Time-Saving | Cuts down the time spent on documentation. |
| Easier Progress Monitoring | Tracks how well interventions are working. |
| Simplified Insurance Claims | Makes claim submissions less complicated. |
| Better Team Collaboration | Ensures everyone is on the same page. |
In multidisciplinary environments, PIE notes act as a shared framework that helps all team members stay informed about a client’s care and progress [2]. The evaluation aspect also allows professionals to assess how well treatments are working and make adjustments based on the documented results [2].
While PIE notes already improve documentation, adding AI tools can take efficiency to the next level – something we’ll dive into in the next section.
sbb-itb-8e8938b
Using AI to Create PIE Notes
PIE notes are becoming a go-to format for mental health documentation, and AI tools are stepping in to simplify the process. These technologies help professionals manage documentation efficiently while adhering to healthcare standards.
How AI Tools Help with Documentation
AI tools bring several useful features to the table, making the documentation process smoother and more efficient:
| Feature | How It Helps |
|---|---|
| Automated Transcription | Converts session recordings into text instantly |
| Smart Formatting | Automatically organizes content into PIE sections |
| Data Integration | Syncs with existing client records seamlessly |
| Quality Assurance | Checks for completeness in documentation |
These tools also work well with existing systems like:
- Electronic Health Records (EHR)
- Telehealth platforms
- Practice management software
- Billing systems
The goal is to create a streamlined workflow that complements current practices while meeting professional requirements [3].
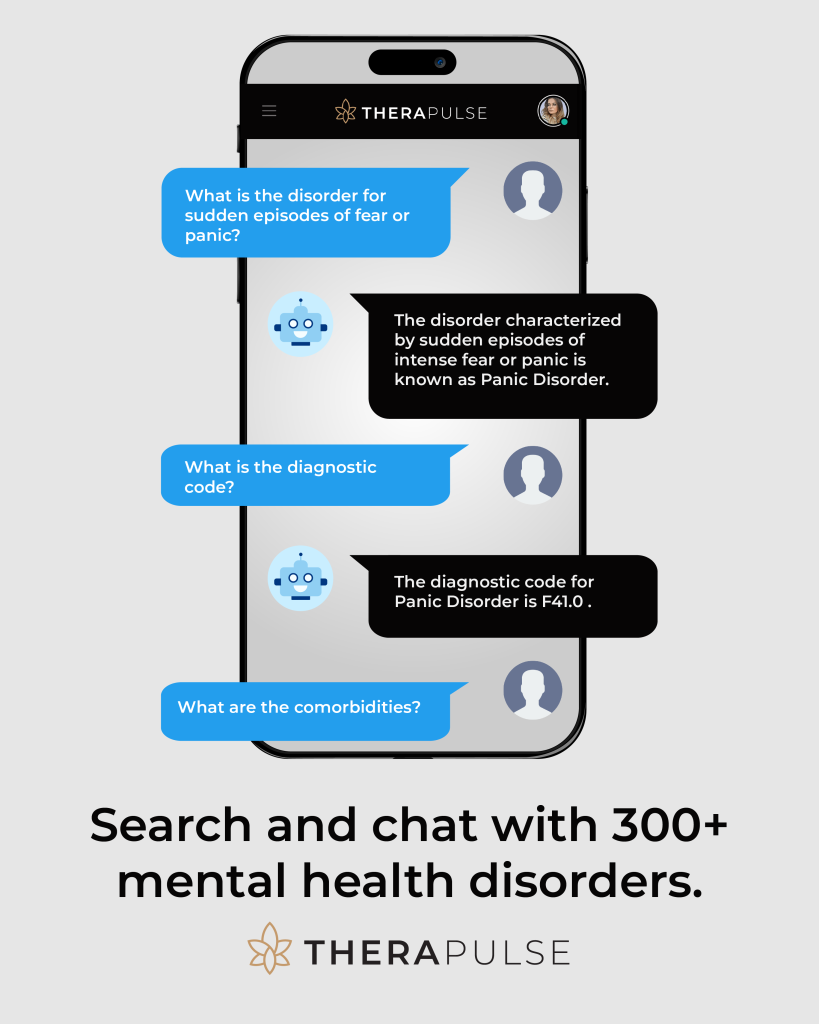
AI Tools for PIE Notes
When choosing an AI tool for PIE notes, mental health professionals should evaluate:
- How easily it integrates with existing systems
- Key features like transcription and formatting
- Security measures for data storage
- User-friendliness and training needs
For example, Therapulse offers automated progress notes with customizable templates and secure storage. It even includes advanced features to analyze clinical data and suggest treatment interventions based on the outcomes documented [3].
AI tools are especially helpful in the evaluation section. They provide insights into treatment effectiveness, enabling professionals to make better decisions about interventions based on the data they’ve documented [3].
Conclusion: Final Thoughts
AI tools are reshaping how documentation is handled, making processes smoother and more efficient. Despite these advancements, structured approaches like PIE notes remain at the heart of effective mental health documentation. By organizing client sessions into Problem, Intervention, and Evaluation sections, PIE notes help professionals create clearer records and improve treatment outcomes.
Modern AI-powered solutions have turned what used to be a tedious task into a streamlined workflow. These tools not only simplify documentation but also uphold high care standards, making professional records more accessible and actionable.
Structured documentation offers benefits that go beyond just keeping records. When mental health professionals use PIE notes effectively, they gain:
| Benefit | Impact |
|---|---|
| Time Management | Cuts documentation time by up to 60% |
| Quality | Ensures all session details are consistently covered |
| Outcomes | Tracks how well interventions are working |
| Compliance | Aligns with professional and regulatory standards |
The combination of AI technology with PIE notes represents a leap forward in mental health documentation. These tools can automate note-taking and offer insights that support better treatment decisions, enabling professionals to stay focused on their clients [3].
As AI documentation tools continue to improve, they promise even greater efficiency and accuracy in mental health care. This ongoing development will further empower practitioners to maintain thorough records while delivering high-quality care [4].
PIE notes remain a cornerstone of effective documentation, offering clarity and actionable insights for better client outcomes. By blending structured methods with advancing technology, mental health professionals can streamline their workflows and continue to deliver outstanding care.
FAQs
How do you write a PIE note?
To write a PIE note, start by clearly describing the problems observed, using factual and concise language. Then, outline the interventions applied during the session. Finally, provide an evaluation of the outcomes and plan the next steps. Write immediately after the session to ensure accuracy and clarity. AI tools can assist in simplifying this process while adhering to documentation standards.
What is the PIE method and model?
The PIE method is a structured approach to mental health documentation, focusing on three main components:
- Problem: The client’s issues and observable challenges.
- Intervention: The actions or treatment strategies implemented.
- Evaluation: The assessment of the results and planning for future steps [3].
This model supports clear and consistent documentation, which is essential for effective treatment planning. It’s widely used in mental health settings to create client-centered records [4].
How does PIE documentation support clinical practice?
The PIE method helps clinicians streamline their documentation while ensuring thoroughness. It allows professionals to:
- Track progress in a structured way.
- Facilitate clear communication within treatment teams.
- Make informed, evidence-based decisions.
- Record outcomes efficiently [5].
By integrating PIE documentation with digital tools, mental health professionals can enhance their workflows and maintain high-quality records [4].
“Mental health documentation is an essential aspect of psychotherapy sessions. Documentation helps mental health professionals track progress from session to session, bill insurance, and helps justify why the client is there” [1].
These FAQs highlight the practical benefits of the PIE method, showing how it supports accurate and efficient mental health documentation.